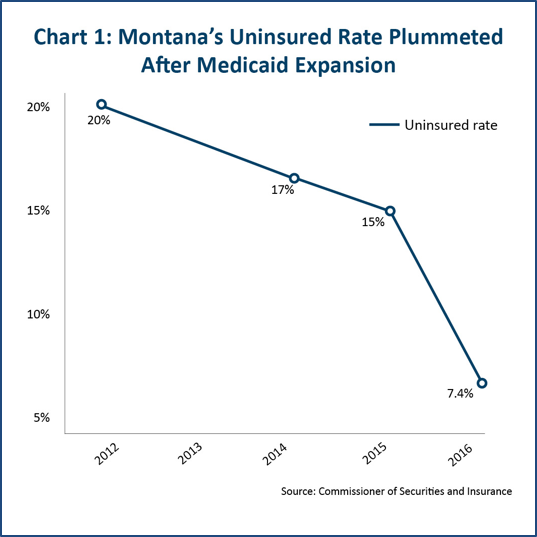
Through access to health coverage under the Affordable Care Act (ACA), Montana’s uninsured rate has dropped from 20% in 2012 to 7.4% in 2016, with thousands of Montanans accessing health coverage through the health marketplace.[i] Congress and President-elect Trump, however, have stated their intent to repeal the ACA in early 2017, without simultaneously putting in place any replacement.[ii] This effort could have disastrous impacts on Montana, leading to 142,000 fewer Montanans with health coverage than if health reform were left in place. At the greatest risk are the over 61,000 Montanans who gained access to affordable health care coverage through Montana’s Medicaid expansion plan.
In the past six years, 12.8 million Americans have gained access to health care coverage.[iii] Repealing the ACA without including a clear replacement that ensures continued access to care poses a significant threat to the economy, and creates uncertainty for millions of Americans.
Montanans Deserve Answers About Future Health Care Coverage
While Congress and President-elect Donald Trump have previously stated their intent to “repeal and replace” the ACA, it appears that Congress intends to move forward with repeal of ACA that will not include a plan for replacement.
Americans have a right to be concerned about the seriousness of plans to put in place any replacement. Since the enactment of the ACA in 2010, Congress has taken over 60 votes to repeal ACA, but it has never voted on any replacement proposal. Repealing the ACA without a replacement plan endangers the health and livelihood of thousands of Montanans.
While this report focuses primarily on the impact of ACA repeal on those who have gained access to coverage through Medicaid expansion – those who are most at risk of losing health coverage – we acknowledge that repeal of ACA also threatens the existing health insurance marketplace that has provided over 52,000 Montanans access to health insurance at more affordable rates, greater consumer protections for those obtaining insurance through employers, and improved coverage for seniors for vital prescriptions drugs through Medicare. These Montanans also face great uncertainties in the future of their health care, without a clear replacement for ACA articulated. Because Congress’ current proposal will repeal ACA without replacement, this report does not take into account the impact of a yet-to-be developed replacement.
Montana Families Face Uncertainty and Disastrous Consequences of ACA Repeal
Prior to the ACA, a staggering one in five Montanans did not have health insurance, with the overall uninsured rate hovering around 20 percent of the total adult population. Today, that uninsured rate has dropped by more than half, to just 7.4 percent, nearly a third of what it was before the ACA (see Chart 1).[iv]
Should Congress repeal the ACA, studies show that approximately 142,000 Montanans would lose health insurance.[v] National studies show that this loss in coverage would occur primarily for families with at least one worker and among individuals without college degrees. Without any of the ACA’s provisions, the number of uninsured Montanans could jump to 227,000.[vi]
Of these 142,000 Montanans losing coverage, 23,000 have accessed subsidies and tax credits to make health insurance more affordable.[vii] In 2016, those that purchased health insurance through the federal health marketplace received an average of $306 in advance premium tax credits, covering 73% of the cost of monthly premiums for insurance.[viii] With the repeal of the ACA, these individuals face the risk and uncertainty of no future financial support to help defray the cost of insurance.
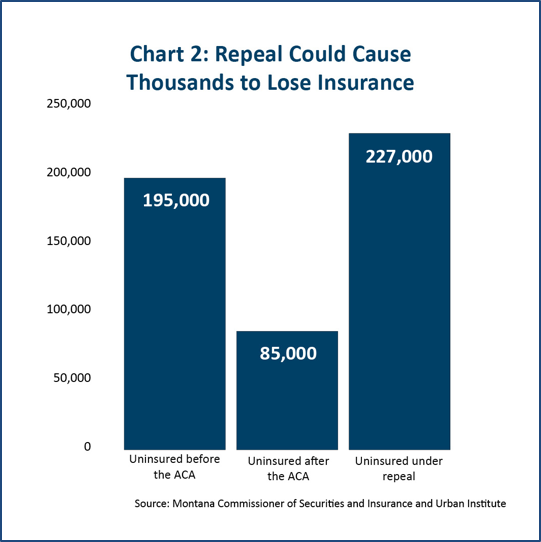
Repeal could cause a greater number of uninsured Montanans than before the ACA was enacted (See Chart 2). In addition to coverage loss to those who have gained insurance through Medicaid expansion, premium tax credits, and cost-sharing assistance, many others face loss of insurance as a result of disruptions in the non-group insurance market.[ix]
With Repeal of ACA, Montana Would Have the Highest Rates of Uninsured Children and Parents in the Nation
ACA repeal could have significant negative impact on coverage of children. Currently, only six percent of Montana’s children are uninsured, but ACA repeal and proposed changes to the Children’s Health Insurance Program (CHIP) could drastically change that. In 2009, the state voted to expand eligibility for CHIP to provide coverage for more low-income children.[x] Today, over 120,000 Montana children receive coverage through Healthy Montana Kids (HMK), with approximately three-fourths of those receiving coverage through Medicaid.[xi]
These rates would be the highest in the nation.
Source: The Urban Institute, December 2016
In each of these scenarios, Montana could face significant budgetary pressures to reduce the number of children eligible for CHIP. According to Urban Institute’s study, a repeal of ACA in combination with reductions in the state CHIP eligibility could result in 41,000 Montana kids losing health insurance, causing the uninsured rate for children to rise to 22.8%.[xiv]
Montana parents would also be at risk under repeal of ACA. Forty-two thousand parents could lose their health insurance, with nearly one in three Montana mothers and fathers going without insurance. This too would represent the highest uninsured rate among parents in the nation. Studies have shown that children’s well being is impacted by their parents’ access to health care, and the consequences of cutting parents’ insurance could be far reaching.[xv]
ACA repeal could also have significant impact on Americans Indians’ access to health services. Repealing Medicaid expansion could jeopardize the improvements Montana has made improving health care access to Indian Country, and put undue strain on health care facilities. Over 8,000 American Indians enrolled in Montana’s Medicaid expansion plan and would be in danger of losing their health care coverage under repeal.[xvi]
Additionally, Congress’ intentions to repeal ACA could put at risk the provisions within the Indian Health Care Improvement Act (IHCIA), included in the ACA in 2010. Under IHCIA, federal and third-party providers are able to now reimburse Indian Health Service (IHS) for services, giving IHS and tribal services much-needed revenue and the ability to expand services.[xvii] Nationwide, reimbursements at IHS facilities, tribal operated facilities, and urban Indian clinics have increased 21% since the expansion of Medicaid.[xviii] In 2014, nearly 40% of American Indians did not have health insurance, but Medicaid expansion represented one of the most significant opportunities to expand coverage for American Indians.[xix],[xx]
The 61,000 Montanans who gained health care through Medicaid expansion are in the greatest danger of losing their health care if the ACA is repealed. By 2019, the year repeal is slated to take place, over 74,000 thousand Montanans could be newly enrolled and in danger of losing their health insurance.[xxi]
Who Might Lose Health Care Coverage?
Of the 61,233 HELP plan members in danger of losing their health care coverage:
· 34,000 are women
· 52,000 are living below the poverty level
· 41,000 are people living at 50% or less of the federal poverty level
· 8,000 are American Indian
· 14,000 are between 50-64 years old
The HELP Plan differs from traditional Medicaid expansion in a few ways, the most significant of which is that a third-party insurance company administers the program. Participants in the program receive health insurance services through the third-party insurance company that covers the same required services as Medicaid does.
· Provides critically needed health care to low income Montanans
· First plan of its sort in the country
· Health care coverage through a third party administrator
· Requires premiums and
co-payments
· Connects participants with jobs and training programs
Montana’s plan also requires HELP Act participants to pay premiums of up to two percent of their income. Participants also pay co-payments, but premiums and co-payments combined cannot exceed five percent of their income. People living above the poverty line may be removed from the program. [xxiv]
The Act also created the HELP-Link program, a voluntary job services program that helps connect program participants with workforce training, employment services and job openings.[xxv] Over 6,500 Montanans have already completed the assessment.[xxvi]
The majority of people who would lose coverage under Medicaid expansion are employed but working at low-wage jobs that do not provide health insurance.[xxvii] Those eligible for coverage through HELP Act include food service employees, cleaning and maintenance service workers, office and administrative support, and construction workers.[xxviii] The vast majority of the people hurt by repeal are people living in poverty: 50,000 Medicaid expansion recipients live below the poverty level, with the other 10,000 living just above it.[xxix]
Veterans and their families are in danger of losing their health care coverage if the federal government withdraws funding for Medicaid expansion. Prior to the HELP Plan, Montana had the highest rate of uninsured veterans (17.3%) in the country.[xxx] Repealing Medicaid expansion could cause approximately 9,500 veterans and family members to lose eligibility for health insurance.[xxxi] While some of these veterans have access to Veterans Affairs (VA) health care, many of them live too far away from a VA hospital or health care clinic to receive adequate care if their Medicaid coverage is taken away.
Medicaid expansion has increased the demand for health care services and supported jobs for doctors, nurses, laboratory technicians, and other medical services staff. With more people employed in the state, and with the newly insured able to spend money at the grocery store that they previously spent on health care, there is more money flowing into the economy and creating jobs. Previous studies on the impact of Medicaid expansion in Montana showed that expanding could create as many as 12,700 jobs, if permitted to continue.[xxxii]
Repealing Medicaid Expansion would cause Montana to lose hundreds of millions of dollars each year in federal funding. In 2019, the first year that repeal of ACA would take full effect, Montana would lose approximately $698 million in federal Medicaid funding. Over the next decade, Montana would lose a total of $9.8 billion in federal Medicaid funding toward health reimbursements to Montana communities and providers.[xxxiii]
The loss of Medicaid expansion funding could have a direct impact on the state’s general fund. By September 2016, just nine months after the Medicaid expansion was implemented, the HELP Act had already saved the state $10.6 million by reducing costs for the Department of Corrections ($1.3 million) and using federal funds to pay for costs that had been covered by the state ($9.3 million).[xxxiv] If ACA were to be repealed, Montana would lose the opportunity for future state savings. In fact, as the uninsured rate grows, this would likely put additional pressure on the state and local governments in additional costs of uncompensated care.[xxxv]
If Medicaid expansion is repealed, Montana hospitals could face significant losses. In 2013, prior to the expansion of Medicaid, Montana’s hospitals incurred $400 million in uncompensated care costs, over half of which was bad debt. People without insurance accumulated most of these costs.[xxxvi] While a full analysis on the impact of Medicaid expansion to providers may not be complete until 2017, initial surveys of Montana’s largest hospitals after the first six months of expansion have shown these hospitals have experienced a reduction in the number of uninsured patients and have seen reduced charity care and bad debt expenses.[xxxvii] Repealing expansion could result in financial trouble for hospitals that would see increases in their uncompensated care.
Montana families and the public deserve to know how a potential repeal will impact their access to affordable health insurance. With little details and the uncertainty of what replacement may be, over 142,000 Montanans are faced with the real risk of losing health coverage. Before Congress votes to repeal the ACA, there must be a clear plan in place that protects all Montanans, including those enrolled in Montana’s HELP plan. A replacement plan that provides inadequate or less affordable coverage would be devastating to the people most in need of health care.
Acknowledgement
The work upon which this report is based was funded, in part, through support from the Montana Healthcare Foundation. The statements and conclusions of this report are those of the Montana Budget and Policy Center.
| Appendix
Table 1: Residents in Every County Could Lose Health Insurance |
|||
| County | HELP Plan Recipients | County | HELP Plan Recipients |
| Beaverhead | 542 | Madison | 232 |
| Big Horn | 1,076 | Meagher | 192 |
| Blaine | 510 | Mineral | 291 |
| Broadwater | 216 | Missoula | 7,457 |
| Carbon | 477 | Musselshell | 405 |
| Carter | 53 | Park | 1,010 |
| Cascade | 5,085 | Petroleum | 20 |
| Chouteau | 243 | Phillips | 269 |
| Custer | 541 | Pondera | 545 |
| Daniels | 43 | Powder River | 39 |
| Dawson | 346 | Powell | 348 |
| Deer Lodge | 582 | Prairie | 32 |
| Fallon | 105 | Ravalli | 2,860 |
| Fergus | 599 | Richland | 371 |
| Flathead | 6,142 | Roosevelt | 1,040 |
| Gallatin | 3,988 | Rosebud | 564 |
| Garfield | 36 | Sanders | 961 |
| Glacier | 1,541 | Sheridan | 118 |
| Golden Valley | 85 | Silver Bow | 2,625 |
| Granite | 121 | Stillwater | 309 |
| Hill | 1,327 | Sweet Grass | 127 |
| Jefferson | 441 | Teton | 414 |
| Judith Basin | 91 | Toole | 218 |
| Lake | 2,397 | Treasure | 31 |
| Lewis and Clark | 3,427 | Valley | 426 |
| Liberty | 186 | Wheatland | 197 |
| Lincoln | 1,619 | Wibaux | 22 |
| McCone | 117 | Yellowstone | 8,174 |

MBPC is a nonprofit organization focused on providing credible and timely research and analysis on budget, tax, and economic issues that impact low- and moderate-income Montana families.