Under the Affordable Care Act (ACA), 41 states, including Montana, have expanded Medicaid to residents with incomes below 138 percent of the federal poverty level, providing significant health and economic benefits to the state. Georgia, however, has taken a different approach - one that has proven to be more costly and has covered far fewer individuals than full Medicaid expansion.
Montana policymakers should be wary of Georgia’s Medicaid model for good reasons. Georgia’s “Pathways to Coverage Program” is a limited expansion of Medicaid that doesn’t work for Georgia, and wouldn’t work for Montana.
Below, we list four reasons Montana should steer clear of this model.
1. Georgians can’t access health care coverage
Limited enrollment in Georgia’s program has been a clear failure for the Peach State. While an estimated 290,000 Georgians qualify for the program, only 4,392 have signed up in the first nine months of the program.
Unlike the states that expanded Medicaid through the ACA, Georgia expanded Medicaid only to individuals living on less than 100 percent of the federal poverty level. This move alone left out thousands of Georgians who would have been eligible under full expansion. The state, however, also added a work reporting requirement - an additional burden not previously allowed under Medicaid.
The requirement to report work hours monthly has burdened many individuals, especially rural Georgians who may not have high-speed internet or lack transportation to a local social services office. Georgia has even subjected full-time parents and caregivers, disabled veterans, and people in full-time residential treatment facilities to this work requirement, effectively making health care inaccessible to many of those who need it the most.
2. Georgia’s model is expensive
Because Georgia did not extend coverage to the entire Medicaid expansion population and created additional barriers for recipients, Georgia forgoes a significant amount of federal funding. In Montana, and in the 40 other states that fully expanded Medicaid through the ACA, the federal government pays for 90 percent of the program cost. This investment of federal funds has resulted in new jobs and millions of dollars in economic activity for the state.
However, under Pathways to Coverage, Georgia is paying a significantly higher portion of costs. The federal government pays for only 66 percent of the costs for Georgia’s new enrollees. If Georgia had adopted full Medicaid expansion, the state would be able to cover nearly half a million residents at a state cost of $496 per individual. Under the current model, however, the state pays five times more ($2,490) to cover each individual.
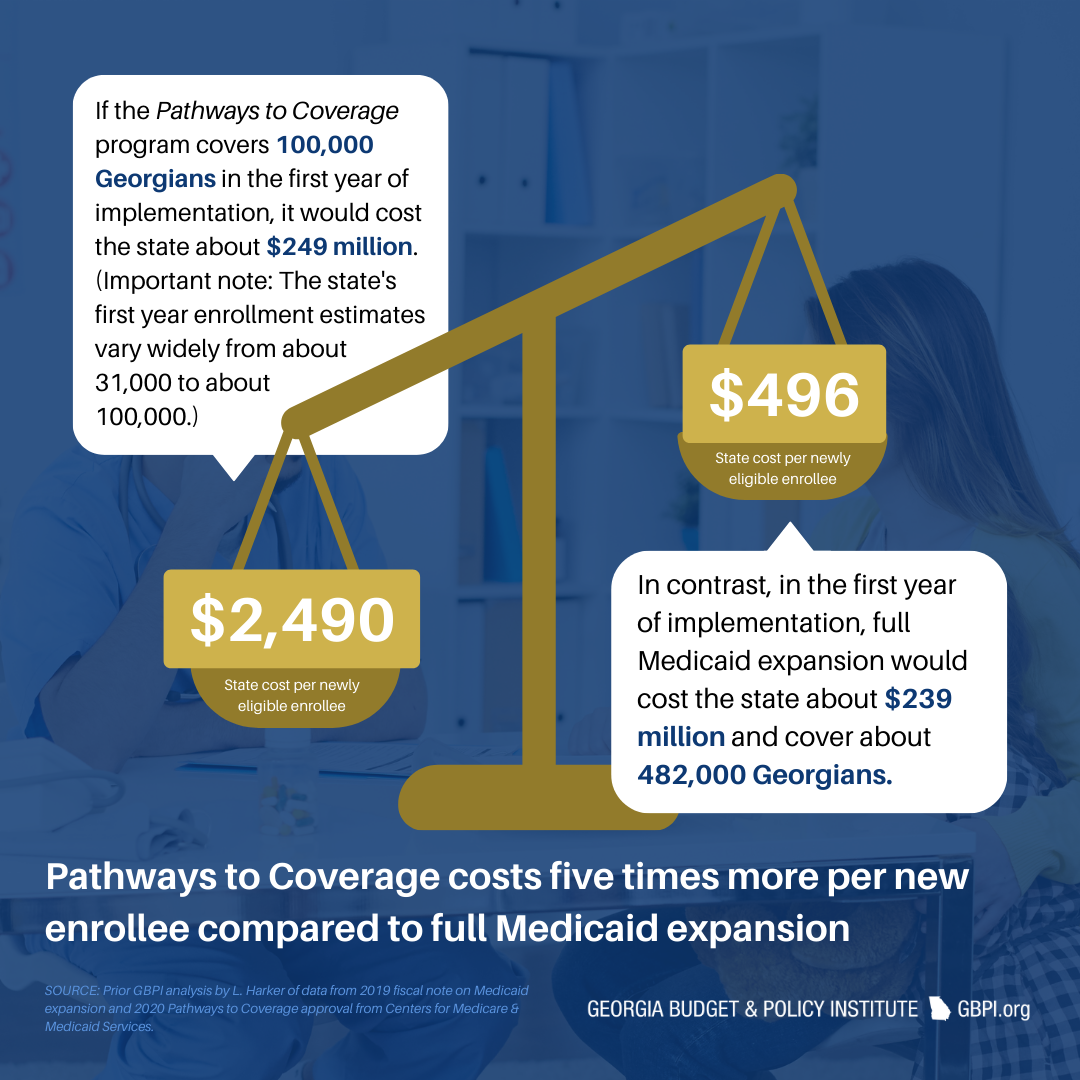
During the first year of enrollment, the Georgia Pathways to Coverage program will cost the state an estimated $249 million if the state meets the projected goal of 100,000 enrollees. Full Medicaid expansion, however, would cost the state less - $239 million - to cover an estimated 482,000 Georgians in the first year of implementation.
So far, the Pathways to Coverage program, with its additional administrative burden of processing work requirements has cost Georgia taxpayers $26 million, with more than 90 percent going toward administrative and consulting costs.
Under the Georgia model, Montana would be stuck paying more to cover fewer individuals. Not only would such a move be morally irresponsible, but it would be fiscally unsound.
3. Most Montanans on Medicaid already work
As we have seen in Georgia, administering work requirements is an expensive use of funds meant to provide health care to individuals, and there is little evidence to support the efficacy of work requirements.
Two-thirds of adults on Medicaid in Montana work, and the vast majority of the remainder report a reasonable impediment to work.
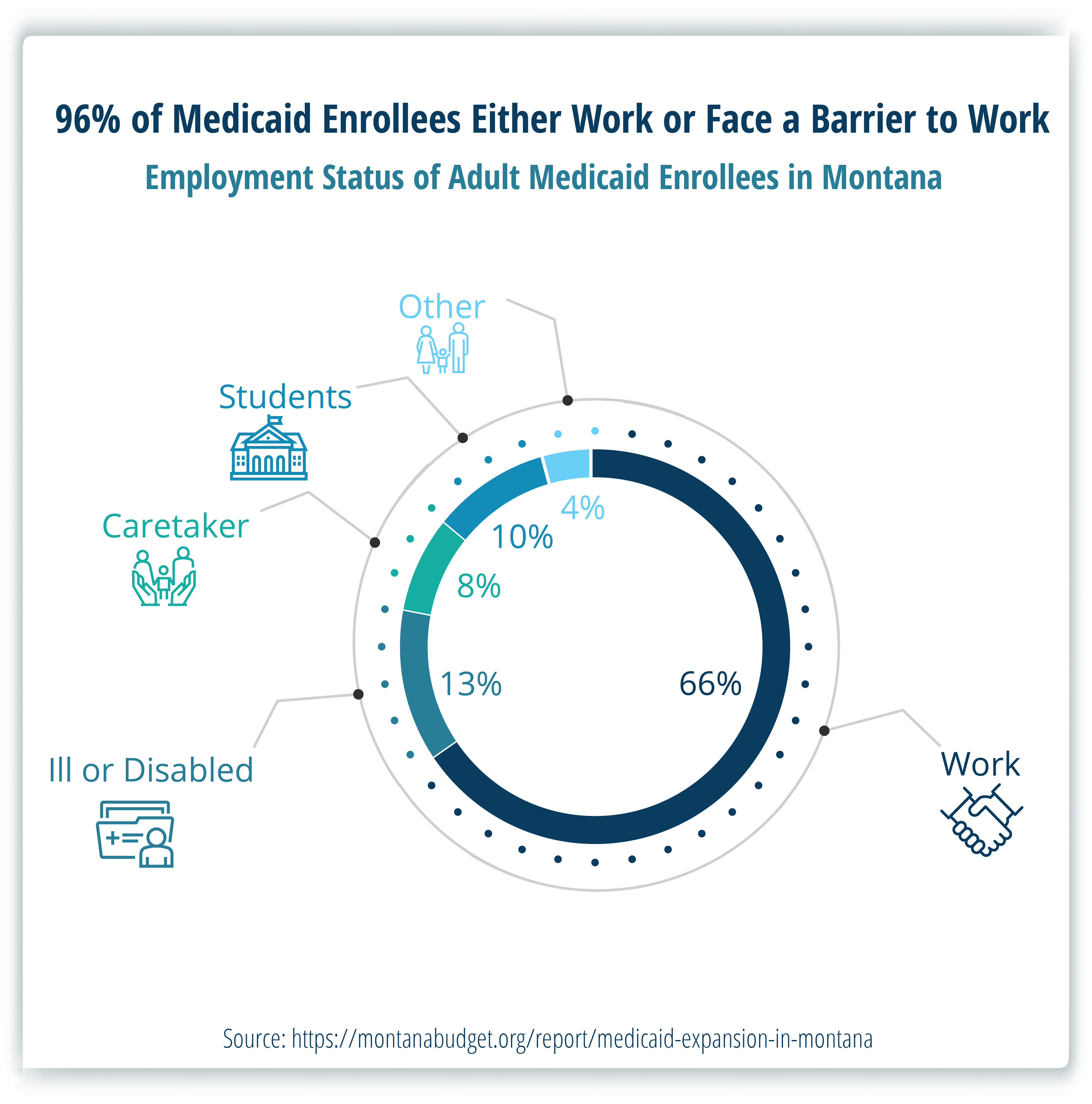
For Montanans who cannot work, due to health, caregiving needs, or other needs, work requirements won’t increase people’s access to work. Instead, they simply serve as an additional barrier to health care for those who need access the most.
4. Montana already has work requirements
In 2019, the Montana Legislature voted to continue Medicaid expansion, albeit with a few changes to the program, including work reporting requirements. However, the federal government never approved these work reporting requirements, and they have not gone into effect. These requirements remain in the legislation and would be enacted if ever approved by the federal government.
Georgia, unlike Montana, had no form of expanded Medicaid coverage when it instituted the Pathways to Coverage program. However, if Montana made changes to its program that hindered access to coverage, it would result in a contraction of the number of participating individuals, rather than an expansion. Thus, it’s unlikely that the federal government would allow Montana to create a similar program.
And for good reason.
Georgia’s Pathways to Coverage model has proven to be inefficient and costly while reaching only a tiny fraction of the population it was meant to serve.
For the last nine years, Montana’s Medicaid expansion program has proven to be reliable and successful, bringing in millions of dollars in federal funding to our health care system, providing jobs, and improving access to care across the state. In 2025, Montana Legislators must again vote to renew Medicaid expansion to keep health care accessible.

MBPC is a nonprofit organization focused on providing credible and timely research and analysis on budget, tax, and economic issues that impact low- and moderate-income Montana families.