Everyone should be able to live a healthy life, but an ongoing history of violent and discriminatory government policies continues to impact the health and well-being of Indigenous people today. These impacts range from poverty rates to Indigenous Montanans having a median lifespan that is a full generation shorter than white Montanans. Indigenous people disproportionately experience lower outcomes across a range of indicators; however, urban Indian people who live away from reservation communities often fare worse. This reality is situated in a history of government policies that aimed to relocate Indigenous people to cities from their Tribal homelands and assimilate them into non-Indian society.
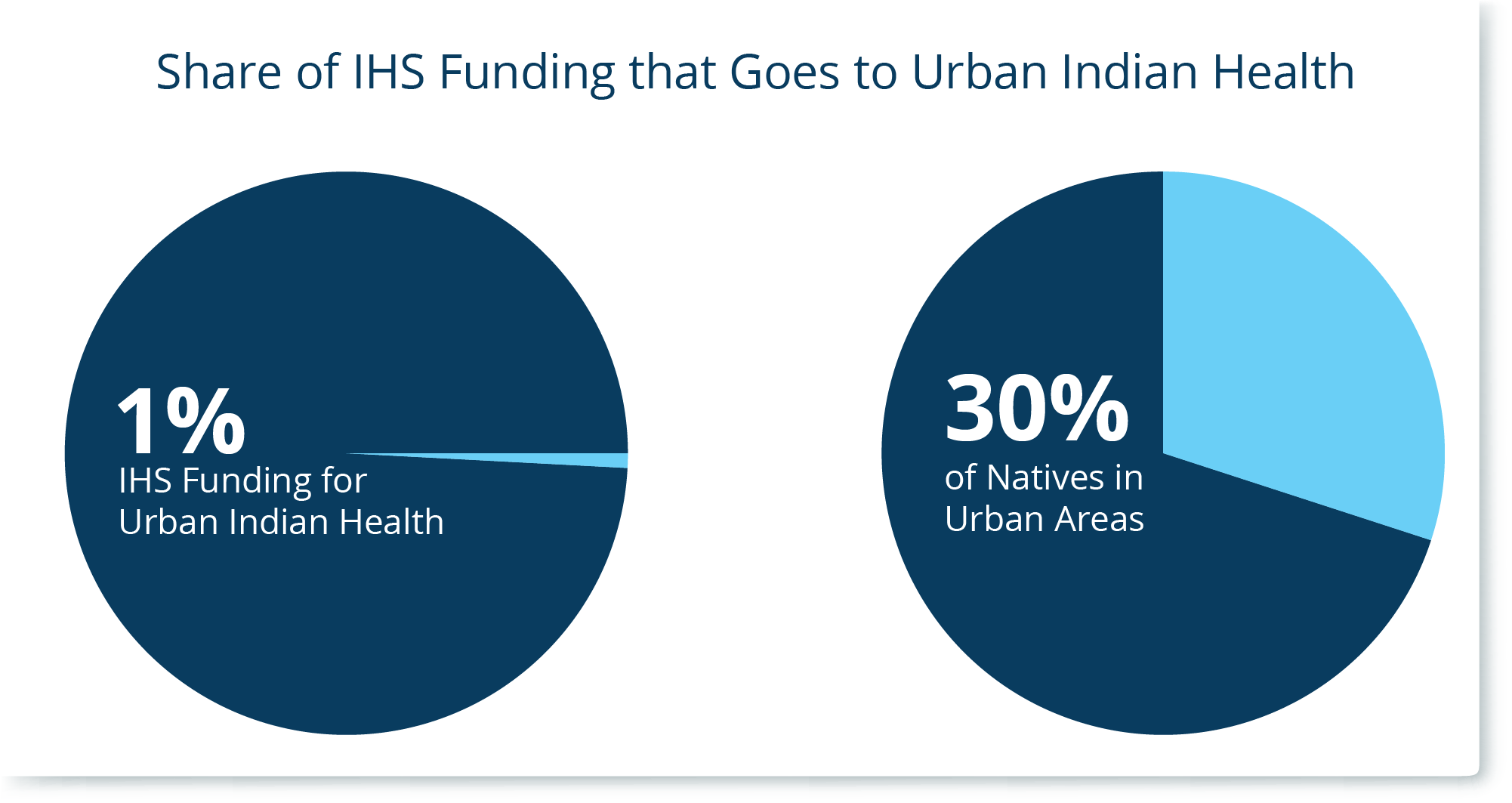
In the wake of these policies, urban Indian health facilities, also known as Urban Indian Organizations (UIOs), emerged to provide urban Indian people with health and social services. UIOs continue to be a critical resource for the communities they serve, including non-Indian people, and they do so on limited budgets. Around one-third (30 percent) of the American Indian/Alaska Native (AI/AN) population lives in a county with a UIO.[1] The federal government holds trust responsibility to provide health services to urban Indigenous people.
 UIO funding accounts for just one percent of the Indian Health Service (IHS) budget.[2] Medicaid makes up around 10 percent of UIO funding. UIOs rely on other limited funding sources to supplement their budget shortfalls.
UIO funding accounts for just one percent of the Indian Health Service (IHS) budget.[2] Medicaid makes up around 10 percent of UIO funding. UIOs rely on other limited funding sources to supplement their budget shortfalls.
While the federal government has a clear role to play, the Montana Legislature has an opportunity to help ensure UIOs have the resources they need to serve Montanans. Three steps the Legislature can take in 2025 include:
Urban Indian Organizations: A Summary
What are UIOs?
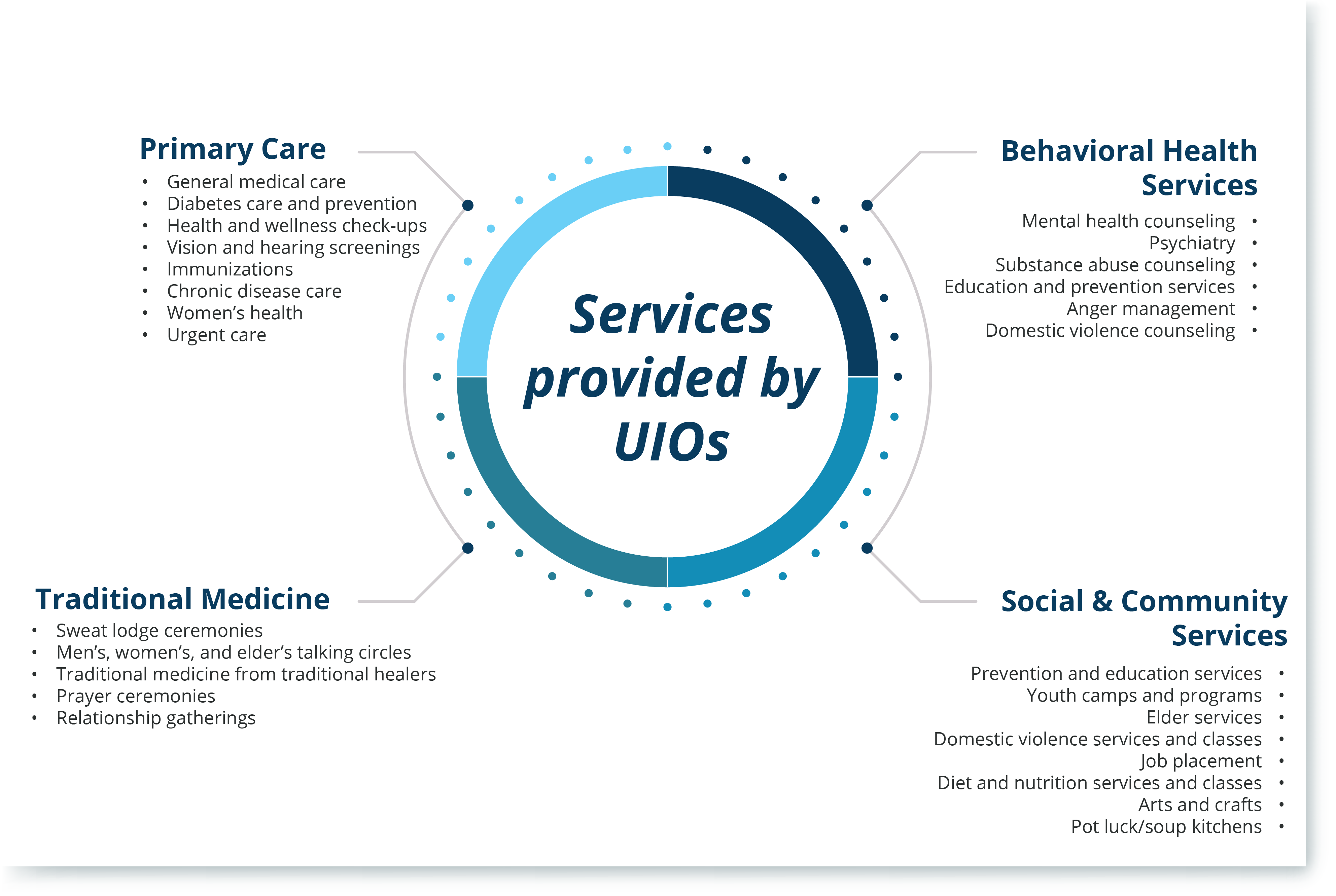
There are 41 UIOs nationwide, five of which are in Montana (Billings, Butte, Great Falls, Helena, and Missoula).[3] Collectively, these nonprofit organizations provide a wide range of health and social services to their communities. UIOs vary in the area they serve, size, the services they offer, and their budgets. While these organizations are diverse, they all commit to providing culturally appropriate services for Indigenous people who may not have access to IHS or Tribal health facilities. UIOs largely fall into one of three service levels:[4]
Who UIOs Serve
While UIOs are committed to serving urban Indian people, they ultimately serve a broader community. Nationwide, UIOs show that around 58 percent of their patient population is non-Indian.[6] Of the 9.7 million Indigenous people in the United States, about 68 percent live on or near their Tribal homelands, leaving around 32 percent in areas not on or near their Tribal homelands.[7] [8] In 2020, 55 percent of the total population served at UIOs were Medicaid beneficiaries, with 46 percent of the AI/AN population served at UIOs being Medicaid beneficiaries.[9] UIOs help serve people who are largely underserved. Across service areas that UIOs serve, Indigenous people younger than 65 are three times more likely than their non-Hispanic white counterparts to not have health insurance (19.7 percent versus 6 percent).[10] The trend holds true for children, with 12.6 percent of Indigenous kids and 3.4 percent of non-Hispanic white kids not having health insurance coverage. Indigenous people overall are nearly three times as likely as non-Hispanic white people to live in poverty (24.5 percent versus 8.9 percent).[11] Research shows a relationship between social disadvantage and poorer health outcomes. Unequal access to education, greater unemployment, higher poverty rates, and housing issues create inequities between urban Indian and white populations.
How They Are Funded
In passing the 1976 Indian Healthcare Improvement Act, Congress recognized the Federal government’s trust responsibility to AI/ANs extended to AI/ANs living in urban areas.[12] However, Federal health care funding toward American Indian and Alaska Native people still focuses largely on Indigenous people living on reservations. While the health care needs of Indigenous people living in reservation communities are significant, about a third of Indigenous people live in urban communities. Despite this and the federal government’s trust responsibility to provide health services to Indigenous people, UIO funding accounts for just one percent of the IHS budget.
In FY 2022, Congress increased urban Indian health spending by 17.13 percent, putting the total at $73.4 million. While it was the highest increase in the past 10 years, this amount falls well below the Tribal Request of $200.5 million.[13]
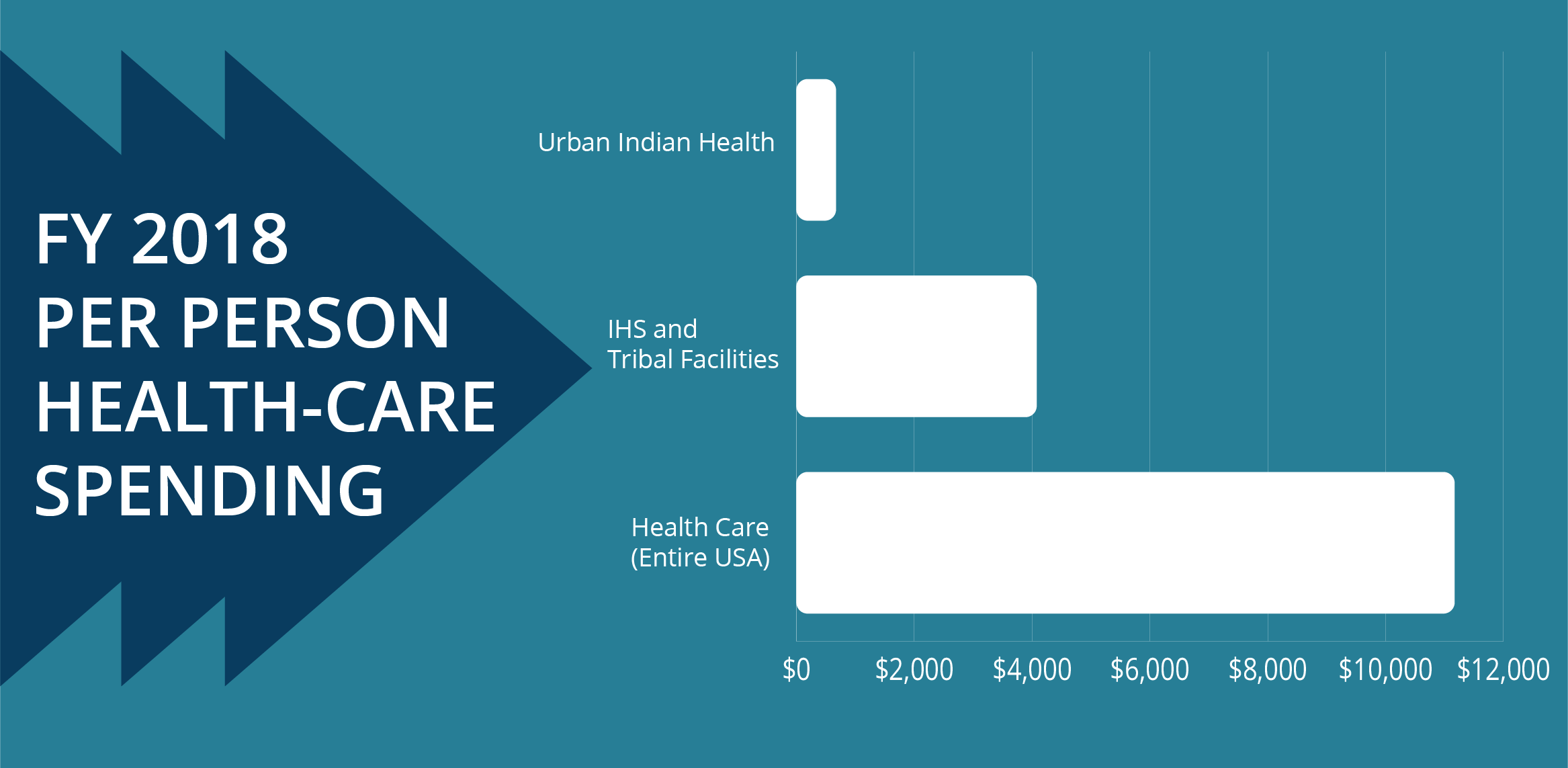
The National Council on Urban Indian Health analysis of FY 2018 appropriations shows that U.S. health care spending per person was $11,172.[14] However, Tribal and IHS facilities only received $4,078 in spending per AI/AN, and spending per person at a UIO showed an even lower amount of $672 from the IHS budget.
The IHS acknowledges that investment in UIOs can improve capacity and access to culturally competent health services.[15] UIOs serve a large share of non-Indian people. By law, UIOs can only use IHS funds to serve Indigenous people. Given inadequate IHS funding and the fact that UIOs must use non-IHS funds to serve non-Indian people, UIOs rely on partnerships with other federal agencies, states, local governments, insurers, foundations, nonprofit organizations, and Tribal Nations that may operate health care programs that receive referrals from UIOs.
Medicaid Expansion
In April 2023, Montana had 20,091 AI/AN Medicaid expansion beneficiaries, with around 32 percent of AI/AN Medicaid expansion beneficiaries residing in a county with a UIO.[16] In 2025, the Montana Legislature must reauthorize Medicaid Expansion. Medicaid has tremendously positive effects on the American Indian population and their healthcare facilities. IHS facilities on reservations have reported expanding services because of expansion. By 2019, seven Tribal Nations expanded from what IHS facilities would classify as Level I (“life or limb”) care to Level IV (preventative services) care.[17] Life-saving preventative care includes prenatal care, mammograms, hip replacements, colonoscopies, and other essential specialty consultations and surgical procedures. IHS facilities receive a 100 percent Federal Medical Assistance Percentage (FMAP) reimbursement, which means any Medicaid-enrolled Tribal citizen attending the facility on the reservation for services will get federal government reimbursement costs at 100 percent.[18] This also means that the state does not have to pay any portion of the costs at that facility. However, for UIOs, Medicaid is reimbursed at the state rates.
The UIOs in Montana worked extensively on Medicaid with the Governor and the Department of Public Health and Human Services to approve their disaster-relief State Plan Amendment (SPA) that increased reimbursement rates for Montana UIOs by 61 percent effective July 1st, 2021, and continued through the end of the COVID-19 Public Health Emergency.[19] The increased reimbursement rates provided Montana UIOs with over $500,000, which is now being invested into establishing a regional behavioral health center. In April 2021, Congress allowed UIOs to receive 100 percent FMAP for AI/AN and non-AI/AN accessing services at their locations.[20] This provision only lasted until March 2023, transferring back financial costs to the state. At a federal level, the state should support UIOs in requesting Congress to reauthorize 100 percent FMAP reimbursements for American Indians at UIOs. The federal government must uphold its trust responsibilities to provide and improve American Indian health care. With continued investments, UIO facilities could thrive by expanding services and community-led programs.
Opportunities for the State to Advance Indigenous Health
While the federal government has a clear role to play, the Montana Legislature has an opportunity to help ensure UIOs have the resources they need to serve Montanans, particularly Indigenous Montanans. Given the fact that the median lifespan of American Indians and Alaska Natives in Montana is about 19 years shorter than that of white Montanans, the state must do more to advance health equity.[21]
Three steps the Legislature can take in 2025 include:

MBPC is a nonprofit organization focused on providing credible and timely research and analysis on budget, tax, and economic issues that impact low- and moderate-income Montana families.